June 26th, 2024
Understanding Topical Steroid Withdrawal (TSW)
I subscribe to many medical and dermatology related newsletters, magazines and informational websites. Medscape Med Pulse, Dermatology Times Magazine, The Dermatologist Magazine from the HMP Global Learning and Skin Healthy Magazine from the American Academy of Dermatology Association are just a few of my favorites. I also read relevant articles from my esthetician magazines and resources; Skin Deep from Associated Skincare Professionals, Dermascope, and Les Nouvelles Esthétiques & Spa magazine. Add in things clients send me from social media like Tik Tok and it’s a wonder I have time in my practice for clients!
But it is critical for me to understand trends, new technologies, and new treatments available. And I do have a tendency to see patterns. An uptick in “rare” cancers being one of them, another one is a rise in social media coverage for Topical Steroid Withdrawal or TSW. Social media is wonderful for many things, however, I have seen a multitude of misinformation on this subject and therefore, felt the need to educate my clients.
TSW is a serious skin condition that should be talked about, and people should be educated on. So what is Topical Steroid Withdrawal?

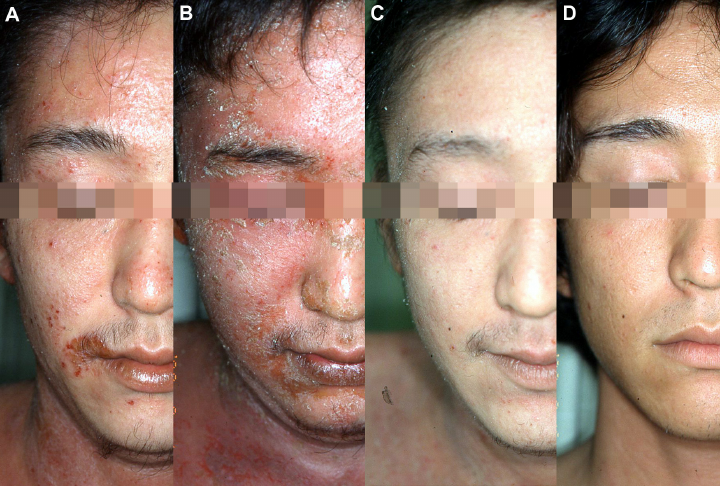
Topical Steroid Withdrawal (TSW), also known as Red Skin Syndrome, is a disease characterized by edema (swelling in skin), erythema (redness in skin), flaking in skin, scab formation and burning sensations in the skin caused by discontinuing prescription medications of mid-to-high potency topical corticosteroids. What makes this so controversial, is the amount of reported dismissal from dermatology healthcare professionals when their patients have experienced symptoms, prompting them to look for help outside of a medical establishment. (1)
Dermatology professionals more often than not will state that it is not the drug that is the cause of TSW, but misuse by the patient. This is clearly stated in the article of Volume 72, March 2015 issue when the conclusion stated, “TCS withdrawal is likely a distinct clinical adverse effect of TCS misuse. Patients and providers should be aware of its clinical presentation and risk factors” as well as cited “low quality of evidence”. (2)
Topical Corticosteroids are prescribed for many different treatments. They are also referred to as glucocorticosteroids and cortisone. They are classified by strength. (See Below List 3)
Class IV Very Potent 600 times as potent as hydrocortisone
Clobetasol Propionate, Betamethasone Dipropionate
Class III Potent 100-150 times as potent as hydrocortisone
Betamethasone Valerate, Betamethasone Dipropionate, Diflucortolone Valerate, Hydrocortisone 17-Butyrate, Mometasone Furoate, and Methylprednisolone Aceponate
Class II Moderate 2-25 times as potent as hydrocortisone
Clobetasone Butyrate and Triamcinolone Acetonide (1% most common strength)
Class I Mild
Hydrocortisone and Hydrocortisone Acetate
So which conditions are these prescribed for and which prescriptions are most common?
Eczema or Atopic Dermatitis– chronic inflammatory skin condition that causes dry, itchy, and inflamed skin. Popular treatments include OTC (Over The Counter) 1% hydrocortisone cream and Eumovate (Clobetasone Butyrate 0.05%) (4) Prescription corticosteroids prescribed could include Fluticasone (Cutivate), Amcinonide (Cyclocort), Betamethasone Dipropionate (Betanate), and Triamcinolone Acetonide (Kenalog). (5)
Psoriasis– chronic autoimmune disorder that causes inflamed, red, raised areas of skin to develop into silvery scales. Popular prescriptions include Clobetasol 0.05% Triamcinolone 0.1% and Hydrocortisone 2.5%. (6)
Lupus- chronic autoimmune disorder, where the immune system mistakenly reacts against your own body, including the skin. This condition is highly inflammatory. Popular corticosteroids prescribed for this condition are hydrocortisone 2.5%, mometasone furoate 0.1%, triamcinolone acetonide 0.1% and a stronger steroid, clobetasol. (7)
Vitiligo– chronic autoimmune disorder, patches of skin lose pigment. In some cases, prescriptions of corticosteroids help slow the progression of vitiligo or allow melanocytes to return, which can lead to repigmentation of the skin. Popular corticosteroids prescriptions include betamethasone, fluticasone, hydrocortisone and clobetasol however most dermatologists will not prescribe this as a treatment if the client has vitiligo on more than 10% of their body and the condition must be non-segmental (the patches appear on both sides of the body). (8)
Contact Dermatitis– happens when the skin comes in contact with a substance that causes an inflammatory skin condition or lesions. This could be by irritant or allergic. Popular corticosteroid prescriptions could include Triamcinolone 0.1% (Kenalog, Aristocort) or Clobetasol 0.05% Temovate or lower potency Desonide ointment (Desowen). (9)
Seborrheic Dermatitis– chronic, non-infectious skin condition that causes scaly patches and dandruff-like flakes. It is thought it may be related to certain autoimmune diseases, nervous system disorders and yeast growth in the skin. Popular corticosteroid prescriptions could include hydrocortisone, fluocinolone (Capex, Synalar), clobetasol (Clobex, Temovate) and desonide (Desowen, Desonate) (10)
Alopecia Areata , Lichen Sclerosus , Bullous Pemphigoid , Aphthous Ulcers are also other disorders that a dermatologist may prescribe corticosteroids for.
Not commonly known, Mycosis Fungoides is a type of rare blood cancer ( cutaneous T-cell lymphoma (CTCL) that occurs when the white blood cells become cancerous. Often, a skin rash is the first sign of this condition, and topical corticosteroids is a possible prescription option along with other oncology therapies.
What Social Media Influencers and Tik Tok Influences Are Not Telling You
Topical corticosteroids are the first line of treatment for many of the above skin conditions for good reason. Dermatologist healthcare professionals have to take into account how severe the disorder or condition is and how aggressive they should treat it.
“Do No Harm” is not just a catchy phrase to use. They have to take into account which treatment is the most effective, while having the least amount of side effects, while also taking into account “how readily available is this treatment for my patient?” and “how affordable is this treatment for my patient?”
Some alternatives to corticosteroids include Dupixent. This drug is used to treat Eczema and Atopic Dermatitis. At the time of this article, the company reported cost to be $3,803.20 USD per carton. Each carton contains 2 pre-filled pens or syringes with needle shields. Each 300 mg pre-filled syringe or pre-filled pen delivers 300 mg/2 mL. Depending on dosage need, that average is a total of $45,638.40 per year without insurance. (11)
Another drug alternative is Cyclosporine, an older drug more commonly known for prevention of organ transplant rejections. Its also known by names Sandimmune, Gengraf and Neoral. These drugs are known to be prescribed for Psoriasis, however there are many side effects that include high blood pressure, short-term and long-term kidney damage and liver inflammation (hepatitis) (12)
Methotrexate is a chemotherapy drug used to treat certain types of cancer (such as acute lymphoblastic leukemia, non-Hodgkin’s lymphoma) that is also used to treat Psoriasis. This is a high risk drug because it may cause lung damage, as well as damage to the lining of your mouth, stomach, or intestines. (13)
(Oral) Rinvoq is a drug used to treat moderate to severe Crohn’s Disease as well as Eczema / Atopic Dermatitis. Studies completed found that this drug caused an increase of the risk of developing non-melanoma skin cancers. Patients were told to avoid the sun and check their skin periodically. (14)
Azathioprine started off as a chemotherapy drug in the 1950’s. Its also known as Imuran or Azapress. (15) This drug is used to treat a variety of disorders including prevention of organ transplant rejection, Crohn’s Disease, and Lupus. This drug increases the risk of developing certain types of cancer, especially skin cancers and Lymphoma. (16)
Compared to the drugs above, the side effects of topical corticosteroids is minimal. Perioral dermatitis (rash around mouth), acne, folliculitis (inflammation of hair follicles), purpura (bleeding from small blood vessels), and contact dermatitis (irritated skin) are some of the most common side effects.
The exact percentage of people who use topical steroids and develop topical steroid withdrawal (TSW) is unknown. There is not sufficient data on that, but what everyone can agree on, is that it is rare considering the amount of topical corticosteroid prescriptions that are prescribed each year.
What these social media influencers are also not telling you is they did not stop their prescription as advised by the health care professional nor did they seek second opinions. Most of the reels and videos I have seen, the social media influencer states that they started to have symptoms, and was prescribed a higher dosage, and the condition worsened but they did not communicate this, or they stopped taking the prescription abruptly. And this goes back to what health care professionals have been grumbling about for over 10 years…misuse of prescription.
How Do You Avoid Topical Steroid Withdrawal
It’s not without saying that I am strictly on the side of all health care professionals. Just like aestheticians, medical professionals have good and bad practitioners. Some will listen and try to find the right course of action, and some are dismissive and are strictly by-the-playbook. But there are things to keep in mind when being prescribed topical corticosteroids. Some things to keep in mind is start off with the lowest potency you can, instead of the highest. Sometimes, less is more. Talk to your healthcare provider about the differences in potency grades and find the right one for you.
Well Directed Treatment Plan: Your healthcare provider should have a clear, well communicated treatment plan. They should not look at your chart for ten minutes, and have the nurse call in a prescription and send you on your way. If you need a stronger potency, grades II or III, then I suggest find a healthcare provider that understands that prescription should be for an average of 14 days and then an office visit to access the condition of the skin. Even better, if possible, use the “Pulse Therapy” method, where topical corticosteroids are used on an intermittent basis rather than continuously.
Observe Skin Changes & Communicate: Only you can give yourself daily attention to your skin and notice any worsening symptoms or adverse side effects. It’s imperative that you communicate with your healthcare provider if there is any changes, keeping in mind that early intervention can prevent the escalation of skin issues.
Discontinuation: When you and your healthcare provider decide to discontinue topical corticosteroids, consider a gradual tapering approach rather than abrupt cessation. This can help minimize the risk of rebound symptoms. (17)
Healing from Topical Steroid Withdrawal
While the lack of research with TSW is concerning, but what we do know is there are stages to healing from this condition. Time frames for healing depend on several factors including the strength of the topical steroids that were prescribed, your skin disorders or conditions that were the reason why you were prescribed corticosteroids, and overall health.
There are stages of healing which are described as inflammation, exudation (formation of pus) and scab formation, proliferation and flaking, and finally repair where the skin is encouraged to produce more collagen, strengthening the skin.
Stages of healing also may not follow the exact sequence and those who are healing could experience flare-ups of the condition. (17)
Topical Steroid Withdrawal can be deliberating, painful and take a long time to heal. Some healthcare professionals report recovery to be from 3 months to 5 years depending on the severity.
As an aesthetician, there is not much within my scope to prescribe to you. I refer out, but work closely as I always do with dermatologists to help you skin heal.
Research & Resources
https://www.pubmed.ncbi.nlm.nih.gov/37119282
https://www.sciencedirect.com/science/article/abs/pii/SO190962214022099?via%3Dihub
https://www.dermnetnz.org/topics/topical-steroid
https://www.eczema.org/information-and-advice/treatments-for-eczema/topical-corticosteroids/
https://www.healthline.com/health/eczema/steroid-cream-for-eczema#side-effects
https://www.goodrx.com/conditions/psoriasis/best-psoriasis-cream
https://www.goodrx.com/conditions/lupus/lupus-rash
https://www.vitiligosociety.org/vitlife/everything-you-need-to-know-about-the-use-of-topical-corticosteroids-for-treating-vitiligo/
https://www.aafp.org/pubs/afp/issues/2010/0801/p249.html
https://www.dupixent.com/support-savings/cost-insurance
https://www.goodrx.com/cyclosporine/cyclosporine-side-effects
https://www.medlineplus.gov/druginfo/meds/a682019.html
https://www.rinvoq.co.nz/rinvoq/safety-information
https://www.medlineplus.gov/druginfo/meds/a682167.html
https://www.tswassist.com/topical-steriod-withdrawel-healing-stages
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4025514
